ISSN: 2206-7418Nanotheranostics
Nanotheranostics 2019; 3(4):331-341. doi:10.7150/ntno.39514 This issue Cite
Research Paper
Microbubble-enhanced ultrasound for the antivascular treatment and monitoring of hepatocellular carcinoma
1. Ultrasound Research Laboratory, Department of Radiology, Perelman School of Medicine, University of Pennsylvania, 3620 Hamilton Walk, Philadelphia, PA 19104, USA
2. Penn Image-Guided Interventions Lab, Department of Radiology, Perelman School of Medicine, University of Pennsylvania, 421 Curie Blvd, 646 BRB II/III Philadelphia, PA 19104, USA
3. University Laboratory Animal Resources, University of Pennsylvania, 3800 Spruce Street, Philadelphia, PA 19104, USA.
4. Department of Clinical Studies, School of Veterinary Medicine, University of Pennsylvania, 3900 Delancey Street, Philadelphia, PA 19104, USA.
*Both authors contributed equally
Abstract
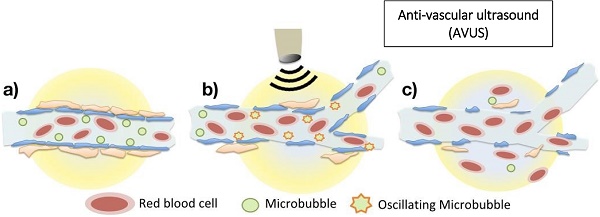
Background and Objective: Hepatocellular carcinoma (HCC) is the most common primary liver malignancy, and its current management relies heavily on locoregional therapy for curative therapy, bridge to transplant, and palliative therapy. Locoregional therapies include ablation and hepatic artery therapies such as embolization and radioembolization. In this study we evaluate the feasibility of using novel antivascular ultrasound (AVUS) as a noninvasive locoregional therapy to reduce perfusion in HCC lesions in a rat model and, monitor the effect with contrast-enhanced ultrasound imaging.
Methods: HCC was induced in 36 Wistar rats by the ingestion of 0.01% diethylnitrosamine (DEN) for 12 weeks. Two therapy regimens of AVUS were evaluated. A primary regimen (n = 19) utilized 2-W/cm2, 3-MHz ultrasound (US) for 6 minutes insonation with 0.7 ml of microbubbles administered as an intravenous bolus. An alternate dose at half the primary intensity, sonication time, and contrast concentration was evaluated in 11 rats to assess the efficacy of a reduced dose. A control group (n = 6) received a sham therapy. Tumor perfusion was measured before and after AVUS with nonlinear contrast ultrasound (NLC) and power Doppler (PD). The quantitative perfusion measures included perfusion index (PI), peak enhancement (PE), time to peak (TTP), and perfusion area from NLC and PD scans. Total tumor area perfused during the scan was measured by a postprocessing algorithm called delta projection. Tumor histology was evaluated for signs of tissue injury and for vascular changes using CD31 immunohistochemistry.
Results: DEN exposure induced autochthonous hepatocellular carcinoma lesions in all rats. Across all groups prior to therapy, there were no significant differences in the nonlinear contrast observations of peak enhancement and perfusion index. In the control group, there were no significant differences in any of the parameters after sham treatment. After the primary AVUS regimen, there were significant changes in all parameters (p ≤ 0.05) indicating substantial decreases in tumor perfusion. Peak enhancement in nonlinear contrast scans showed a 37.9% ± 10.1% decrease in tumor perfusion. Following reduced-dose AVUS, there were no significant changes in perfusion parameters, although there was a trend for the nonlinear contrast observations of peak enhancement and perfusion index to increase.
Conclusion: This study translated low-intensity AVUS therapy into a realistic in vivo model of HCC and evaluated its effects on the tumor vasculature. The primary dose of AVUS tested resulted in significant vascular disruption and a corresponding reduction in tumor perfusion. A reduced dose of AVUS, on the other hand, was ineffective at disrupting perfusion but demonstrated the potential for enhancing tumor blood flow. Theranostic ultrasound, where acoustic energy and microbubbles are used to monitor the tumor neovasculature as well as disrupt the vasculature and treat lesions, could serve as a potent tool for delivering noninvasive, locoregional therapy for hepatocellular carcinoma.
Keywords: Hepatocellular carcinoma, noninvasive cancer therapies, antivascular ultrasound, preclinical studies
